Bone marrow transplantation is a medical procedure that involves the replacement of damaged or diseased bone marrow with healthy bone marrow stem cells. This procedure is used to treat several illnesses, including leukemia, lymphoma, and aplastic anemia, among others. The success of bone marrow transplantation depends on many factors, including the compatibility of the donor and the recipient, the type of transplantation, and the health of the patient before and after the procedure. In this blog post, we will discuss bone marrow transplantation and the unique challenges and considerations for BONE MARROW TRANSPLANTS & LGBTQ+ individuals.
What is bone marrow transplantation?
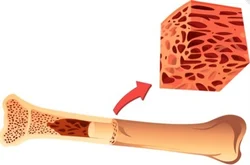
Bone marrow transplantation (BMT) or hematopoietic stem cell transplantation (HSCT) involves the removal of stem cells from a donor’s bone marrow or blood and their transfer to a recipient. The stem cells can be obtained from the patient, called autologous transplantation, or from a donor, called allogeneic transplantation. The cells are transferred to the recipient through a needle inserted into the bone, where they will settle and stimulate new bone marrow cell growth.
The primary use of a BMT is to replace dysfunctional or damaged bone marrow with healthy cells that can produce all types of blood cells. The recipient’s immune system may attack the donor cells, causing a condition called graft-versus-host disease (GVHD). This condition can cause the recipient’s body to reject the transplanted cells, leading to serious complications and increased hospitalization.
Another development in the field of BMTs is the use of cord blood for transplant. Cord blood is a source of hematopoietic stem cells that are derived from the umbilical cord and placenta after childbirth. In the past, this blood was otherwise thrown away as medical waste, but now, it’s being collected and stored for future use in transplants. Cord blood transplants offer patients more viable options for transplant donors, especially those from underrepresented backgrounds. The process of cord blood transplant is also less complicated than bone marrow transplantation, reducing the risk of complications during the procedure.
Challenges and considerations for BONE MARROW TRANSPLANTS & LGBTQ+ individuals
The LGBTQ+ community faces several unique challenges when it comes to healthcare. These challenges include lack of understanding and discrimination, among others. Although bone marrow transplants may not seem directly connected to LGBTQ+ individuals, these community members face some unique considerations when it comes to transplantation.
Lack of representation
One of the most common challenges that LGBTQ+ individuals face is a lack of representation in the medical community. This lack of representation means that sometimes there’s no concept of their unique experience of being trans or queer. The procedures and tests that were designed to work for the mainstream may not accurately apply to the LGBTQ+ community. When you consider bone marrow transplantation, this lack of representation can be critically important. Bone marrow typing data depends on the patient’s blood type and the antigens that are part of their tissue type. While most research focuses on heterosexual donors and recipients, there is limited data available for donors and recipients who are part of the LGBTQ+ community.
Transgender individuals
For transgender individuals who have undergone hormone replacement therapy (HRT), they may need to pause their therapy to ensure that HRT does not have any harmful effects on the transplantation process. This can be a daunting task because it can mean that their transition will be paused, which may be frustrating, demoralizing, and a risk to their mental health. The main concern with HRT is whether it will interfere with the patient’s immunosuppressants. Because immunosuppressants play a crucial role in bone marrow transplantations, and interaction with other medications may lead to complications, it’s essential to minimize all possible interactions. The lack of research in this area produces limited evidence.
LGBTQ+ community members are more likely to experience mental health problems.
One significant challenge associated with bone marrow transplants is the emotional, mental and physical toll it takes on recipients. LGBTQ+ individuals, in particular, are more prone to mental health problems, such as anxiety and depression. Furthermore, studies have shown that LGBTQ+ community members have elevated rates of substance abuse and suicidal ideation. For this reason, healthcare providers need to be mindful, intentional, and well-trained in how they approach mental health concerns, especially for marginalized communities.
Gestational aspect
Another lesser-discussed aspect of bone marrow transplantation is the possibility of gestational problems, specifically for transgender donors. If a transgender woman requires BMT, she may have to halt hormone therapy to preserve sperm to have biological children in the future. The same risk exists for transgender men since discontinuing testosterone for an extended time can lead to problems with fertility. The thought of halting hormone therapy for a bone marrow transplant to allow for the possibility of having biological children is challenging for transgender individuals, and practitioners must be prepared to engage and support them through the decision.
The importance of empathetic care
There are several challenges when it comes to conducting bone marrow transplantations on the LGBTQ+ community. Lack of representation, mental health problems, and gestational concerns are a few of the factors healthcare providers should address. However, a robust support system can make all the difference in providing compassion and care to members of the community.
To provide appropriate care, healthcare providers must acknowledge the unique issues that LBTQ+ community members may face. It can help by seeking opinion from other experts who have studied transgender patients receiving chemotherapy for cancer. Listening to concerns, promoting open communication channels, and providing non-judgmental, empathetic care services is crucial. Having a supportive healthcare provider will build a strong therapeutic relationship and safety net for the LGBTQ+ recipients, which will contribute to a positive transplantation experience.
Conclusion
In conclusion, bone marrow transplantation is becoming more common, but transplants carry those experiencing them through an emotional rollercoaster. The process of bone marrow transplantation can be challenging to anyone, and providers must appreciate and support individuals from the LGBTQ+ community through the process. The challenges range from physical health challenges such as the impact of hormone therapy to mental health challenges. To better care for members of the LGBTQ+ community, healthcare providers need to take a holistic approach, understanding and addressing these challenges with sensitivity and empathy. The importance of building therapeutic relationships with patients can not be overemphasized. By providing more comprehensive services, healthcare providers can ensure that bone marrow transplantations can be successful for anyone who will benefit from the procedure.