Bone marrow transplants (BMTs) are a powerful tool for treating a range of conditions, including leukemia, lymphoma, and other types of cancer. However, access to this life-saving treatment is often limited by health disparities that disproportionately affect people of color and low-income communities.
In this post, we will explore the issue of health disparities in BMTs, discussing the challenges that individuals and communities face in accessing and receiving adequate care, as well as ways to address these disparities and improve outcomes for all patients.
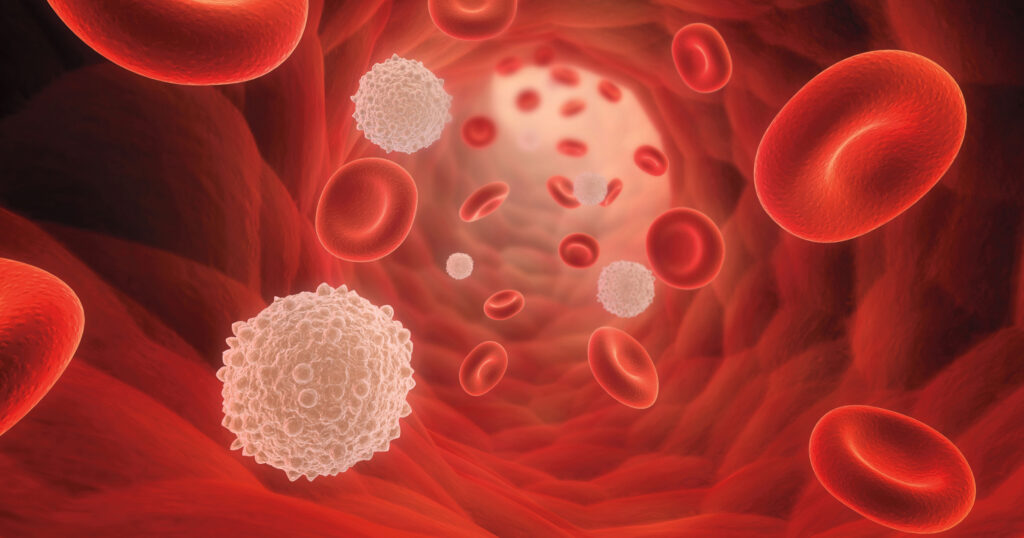
There are two main types of bone marrow transplants: autologous and allogeneic. Autologous transplants involve collecting a person’s own bone marrow or peripheral blood stem cells, freezing them, and then reinfusing them back into the person’s body after they have undergone high-dose chemotherapy or radiation. This type of transplant is used to treat some types of lymphoma and multiple myeloma.
Allogeneic transplants, on the other hand, involve using bone marrow or stem cells from a donor, either from a family member or an unrelated person. Before the transplant, the recipient undergoes high-dose chemotherapy or radiation to destroy their own bone marrow and suppress their immune system, which helps to prevent rejection of the donor cells. After the transplant, the donor cells engraft in the recipient’s body and begin producing new, healthy blood cells.
Health disparities refer to differences in health outcomes or access to health care that are influenced by social, economic, and environmental factors. These disparities can have a significant impact on individuals and communities, leading to higher rates of illness, disability, and premature death.
There are many different factors that contribute to health disparities, including race, ethnicity, socioeconomic status, gender, sexual orientation, and geographic location. People from marginalized communities often face challenges in accessing quality health care, as well as barriers to healthy living, such as lack of access to healthy food, safe housing, and quality education.
There are several ways in which health disparities can impact access to and outcomes of bone marrow transplants. One key factor is the availability of donors. According to the National Marrow Donor Program (NMDP), individuals of African descent have a lower likelihood of finding a matching donor than individuals of European descent. This is because the markers used to match donors and recipients are based on genetic ancestry and differ between different racial and ethnic groups.
Another factor that contributes to health disparities in BMTs is the cost of the procedure. Bone marrow transplants can be extremely expensive, with the average cost ranging from $200,000 to $400,000. While insurance typically covers a portion of the cost, patients are often responsible for significant out-of-pocket expenses, including copays and deductibles. This can be a significant barrier for individuals and families with limited financial resources.
Addressing health disparities in bone marrow transplants requires a multi-faceted approach that addresses structural barriers to access, improves the quality of care provided to all patients, and supports research and advocacy aimed at advancing health equity.
One key strategy for improving access to bone marrow transplants is to increase the availability of donors from diverse racial and ethnic backgrounds. This can be achieved through targeted recruitment efforts, as well as increasing awareness of the importance of bone marrow donation among individuals from underrepresented communities. Efforts should also focus on reducing the financial burden associated with BMTs, such as by expanding insurance coverage or providing financial assistance to those in need.
Improving the quality of care provided to all patients requires addressing systemic biases in the healthcare system, as well as ensuring that patients have access to culturally competent care that is tailored to their individual needs and preferences. This may involve providing training for healthcare providers in cultural competency, unconscious bias, and equity, as well as providing resources and support for patients and families to help them navigate the complex healthcare system
Finally, advancing equity in BMTs requires investing in research and advocacy efforts that aim to identify and address the root causes of health disparities. This may involve supporting research into the underlying biology of different diseases and their impact on different patient populations, as well as advocating for policy changes that promote health equity and access to quality care for all.
Bone marrow transplants are a powerful tool for treating a range of cancers and genetic disorders, but access to this life-saving treatment is often limited by health disparities that disproportionately affect people of color and low-income communities. Addressing these disparities requires a multi-faceted approach that focuses on increasing access to donors, reducing the financial burden of BMTs, improving the quality of care provided to all patients, and investing in research and advocacy aimed at advancing health equity. By working together to address these challenges, we can ensure that all patients have access to the lifesaving treatments they need to live healthy and fulfilling lives.